Annual Report
2021-2022
Welcome
On 7 June the Pae Ora (Healthy Futures) Bill passed its third reading in Parliament, marking a significant milestone in the Government’s commitment to delivering a better health system for Aotearoa New Zealand. The Bill is part of a health system reset. On July 1 it will establish Te Whatu Ora and the Te Aka Whai Ora as permanent entities to replace DHBs, establish the public health agency within the Ministry of Health, and strengthen the stewardship role of the Ministry of Health.
The landmark reforms enshrine the Te Aka Whai Ora as an equal partner at the heart of the new health system, empowering it to co-commission and plan services across the system in conjunction with Te Whatu Ora, commission its own kaupapa Māori services, and monitor the performance of the health system for Māori.
In addition to the Te Aka Whai Ora, Iwi Māori Partnership Boards will ensure that the voice of whānau is heard and helps shape health services delivered locally, so that they better reflect those who need and use them.
In April, the Government announced the first nine locality network pilots to improve how healthcare is delivered in local communities, including a pilot in the Eastern Bay of Plenty. WBOPPHO chief executive Lindsey Webber says the reforms are game changing for both the health sector and local communities who will benefit from equity focussed strategies.
“The change means we farewell what we know as the Bay of Plenty DHB, whose partnership we’ve greatly valued over the years.”
Organisational changes in recent months have positioned the PHO to make the most of opportunities within the changing health landscape, she says.
“We are even more focussed in our mahi to address inequities for Māori and harness the strength of population data to deliver services that have a positive impact on the health and wellbeing of our communities.
“What’s more, our connections with iwi, the General Practice network, and other providers demonstrate our proven track record in working collaboratively to achieve improved health outcomes for everyone.
“As a PHO, we’re excited to see the first pilots established and look forward to playing a role in the new locality-based delivery model as it takes shape.”
Contents

The Western Bay of Plenty Primary Health Organisation Co-Chairs, Paora Stanley and Dr Daniel McIntosh.
Co-Chair’s Report
As we move towards a time that seems to hold hope and room to refocus on non-COVID related health goals, we are in no shortage of challenges. But what we have shown is that as a united community of health providers, iwi, support staff, and clinicians, we have the resilience, ideas, innovation and collaborative spirit to change and adapt, to solve and grow.
Health reforms are at the forefront of our minds, bringing change to the sector that will require this collaborative spirit for which the Western Bay of Plenty Primary Health Organisation has become known.
Chief Executive Officer’s Report

Shared partnerships and values pave the way
If there’s one positive thing going through the last few years of the pandemic achieved, it was to shine a light on the far-reaching and successful impact of collaboration. It was to show that we can quickly and meaningfully come together across disciplines and health services, sharing resources and knowledge with local iwi and many other providers, to address the most complex of health and wellbeing issues.
You’ll see that throughout the year as a PHO we’ve been continuing to address COVID as everyone else has, but the benefits that have resulted through this mahi are the meshing of expertise, discipline, passion, and understanding. We have continued to actively and purposefully strengthen these bonds and relationships to create long-term goals, plans, and initiatives that will start to reach some of the most marginalised and vulnerable in our region.
This takes time, trust, and tenacity. As a PHO we have these in spades and our annual report reflects the mahi involved. I am immensely thankful to and proud of the PHO kaimahi for their commitment and dedication to our kaupapa.
With the health reforms gaining pace, a series of district, regional and national huis are providing opportunities to share thoughts and ideas to inform locality development and explore our role in shaping the future of primary health.
Our Practices
Bethlehem Family Doctors
Bethlehem Medical Centre
including
Omokoroa Medical Centre
Chadwick Healthcare Limited
including
Chadwick Bethlehem
Chadwick Greerton
Chadwick South City
Chadwick Tauriko
Cicada Health
Dee Street Medical Centre
Epic Health Medical Practice
Family Doctors
including
Brookfield
Pyes Pa
The Lakes
Farm Street Family Health Centre
Fifth Avenue Family Practice
including
5th Ave on 10th
Gate Pā Medical Centre
Girven Road Medical Centre
Hairini Family Health Centre
Healthcare on Fifteenth
Katikati Medical Centre
Mount Medical Centre
Ngāti Kahu Hauora
Ōtūmoetai Doctors
Pāpāmoa Beach Family Practice
Pāpāmoa Pines Medical Centre
including
Pāpāmoa Pines @ Palm Springs
Pāpāmoa Pines @ Whitiora (opened October 2022)
Poutiri Wellness Centre
Tara Road Medical Centre
Te Puke Medical Centre
Te Puna Doctors
The Doctors Bayfair and Pāpāmoa
The Doctors Bureta
The Doctors Kopeopeo
The Doctors Phoenix
The Doctors Tauranga
The Doctors Total Health
The Doctors Welcome Bay
Third Age Health (Tauranga)
Our Population
Working alongside our General Practices and Iwi, Western Bay of Plenty Primary Health Organisation supports healthy lifestyles and quality healthcare services for a growing number of people in our local communities.
82.9%
+ 3,785
+1.9%
Our PHO population growth exceeds the 1.63% estimate for the Bay of Plenty region and is above the 2020 national average of 1.31%.
Western Bay of Plenty PHO currently serves 83% of the estimated population living within the Bay of Plenty. Residents are dispersed from Waihī in the west to Whakatāne in the east. 15.8% of these identify as being Māori and a further 1.7% as Pasifika. People who identify as Asian accounts for 7.5% of our enrolled population.
Net growth in enrolments at General Practice averaged 315 per month over the past year (376 in 2021).
with General Practice
+ 57,351
+ 839
+6.7%
Increase in Māori enrolments this year
with General Practice
+ 16,700
+ 964
+2.2%
Increase in over 65 years enrolments this year
21.9% of the enrolled population
+2.8%
Increase in Pasifika enrolments this year
+6.9%
Increase in Asian enrolments this year
+0.6%
Increase in Under 14s enrolments this year
88.8%
$44.61m
Funding received on behalf of General Practice in the year ended 30 June 2022 for the enrolled population.
Funding received on behalf of General Practice was $41.61m in the year ended 30 June 2022 for the enrolled population. This funding is used to provide services that promote population wellbeing and management of personal health.
Other targeted funding is received to enable clinical programmes and interventions to address specific areas of primary health care.

Māori Health Planning and Iwi Partnerships
Our commitment
Our priority is to improve Māori health and wellbeing as we strive to be courageous leaders of compassionate, connected, trusted and innovative whānau-centred healthcare provision for our whole population. Bridging health inequities is the driving factor of our organisation and is at the heart of what we do. Our team is dedicated to serving the community and creating health equity for all. We stride forwards by embracing locality models, with the knowledge that it’s the people on the ground within the community who will help us make a real difference.
Committed to ensuring pro-equity performance measures are embedded in all PHO programmes and contracts and across all operational functions, read our stories below to find out more about how we have embraced locality models and partnered with health and community focused initiatives to achieve health equity for all.

Data driving efficiency and equity
Improvements to data reporting over the past 15 months have made it easier for the PHO and General Practices to tap into information to drive health improvements, business efficiencies, and to narrow the equity gap between Māori and non-Māori patients.
- All network practices have benefited from the improvements, with those participating in the Health Care Home (HCH) model able to access data intelligence and trend analysis reports to fine-tune how they care for patients and whānau, and to demonstrate the value of the HCH model.
- Reports are now more reliable, reproducible, and relevant, meeting the Te Whatu Ora contract and national standards for HCH reporting.
- Population and performance data reporting systems developed.
- A deliberate focus taken to provide reporting that supports efforts to address inequities. Achieved by applying an equity lens to the work to enable reporting on Māori and non-Māori population data. This data is now routinely extracted from the Patient Management Systems to report the disparity that exists between these populations.
- New dashboard-style reporting and better systems developed to make sense of the complex data streams sourced from various platforms across the regional health network.
- Data feeds set up to connect with Thalamus, the online reporting platforms used by practices, for more cohesive and insightful overviews. Manual queries have also reduced.
- The real-time data now available is a game changer for practices, with numerous applications that support proactive and preventative care, including post-discharge care to reduce readmission rates. Practices can also now go online and see, in real-time, their patients’ presentations, admissions, and discharges from hospital.
- The new data improvements allow more precise performance measurements against targets.
PHO health promotion coordinator and member of the Western Bay of Plenty Smokefree Coalition, Tiana Bennett.
Educating community on smoking law change
To reduce children’s exposure to second-hand smoke, from 28 November 2021 it became illegal to smoke or vape in a vehicle that has children under 18-years-old in it, whether the vehicle is moving or not. The Western Bay of Plenty Smokefree Coalition and our local primary health network created a campaign to educate communities about the law change and encouraged people to avoid smoking and vaping inside a vehicle by adopting practical steps to change their behaviour.
PHO health promotion coordinator and Coalition member Tiana Bennett said while many smokers agreed with it, there were still some people struggling to make the transition to a smokefree car.
The coalition, with support from Waipu Hauora at Matapihi, distributed ‘Drive Smokefree for Tamariki’ campaign resources to targeted communities, including kura kaupapa Māori, whānau at kōhanga reo, and 25 other hauora across Tauranga Moana.
Tiana says the proposed laws would be supported by a new Smokefree 2025 Taskforce and an increase in the number of smokefree enforcement officers.
“It is ground-breaking for Māori, as it will create a smokefree generation whereby our tamariki and our mokopuna will never smoke.”
Campaign snapshot
Resources distributed included posters, car air fresheners, and bumper stickers.
- People submitted photos of their stickers and air fresheners on display to win petrol vouchers.
- Efforts were focussed on educating rangatahi (young people) about the new legislation.
- Information was provided to young people who attended a careers information night at Huria Marae, while rangatahi were also encouraged to show their support for the campaign by sending in TikTok videos to win a prize.
- Māmā taking part in the PHO’s Hāpai Pēpi sessions also took part.
- Using social media and involving the younger cohort, in particular, helped us to generate a lot of support for the smokefree kaupapa.
Te Puke High School teachers (from left) Ray Ryan, Sophie Mercer, Ivan Munkedal, Tayla Toma and Kamal Nair, raised the most money as a team.
Mauri Ora: Inspiring positive health changes
Māori tāne (men) shared their stories of resilience and hope at an iwi-led event organised to celebrate their achievements in reaching their fitness and fundraising goals. The December 2021 event at Fraser Cove capped off a month of activities and encouragement led by Mauri Ora coordinator Te Aihe Toma in support of men’s health charity Movember.
A total of $10,000 was raised by the individuals and groups who signed up to support the Mauri Ora challenge, Hurungutu. Te Aihe says the commitment and discipline from Movember participants in 2021 was outstanding.
“We had groups from all over the Western Bay of Plenty, including staff from Ngāti Ranginui Iwi Society, join in on the kaupapa of Movember,” says Te Aihe.
“People could take part in the official Mauri Ora activity challenge or get involved by donating money or simply growing a moustache.
“Everyone had their own motivations for participating, and what was so rewarding was seeing people smash their personal goals and share with whānau and team members their health experiences, either good or bad. It’s about encouraging men to have those conversations and be there to tautoko (support) them.”
Teams and individuals were awarded prizes, with the event also a chance for men to share their personal health struggles.
The Western Bay of Plenty PHO has funded the Mauri Ora programme since 2016.
Individuals bravely shared their stories at the iwi-led Mauri Ora event to encourage others.
John Brown, 44, and Jack Te Moana, 52, both battled bowel cancer and shared how they had initially delayed seeking treatment after experiencing symptoms.
“My father died of cancer in 2020 then I started experiencing my own symptoms in May, but I put off seeing the doctor,” says John.
“Eventually my wife persuaded me to have a colonoscopy and the doctors caught it in the nick of time.”
He had surgery last year to remove a portion of his bowel. Jack experienced bowel pain last summer, but ignored it, choosing to spend time with whānau over the holidays.
“Then my aunty died of cancer and the week we buried her was the week I found out I had bowel cancer. My experience has made more of my family get checked.”
Brandon McIndoe, 23, shared his mental health struggles and says he used fitness as part of his strategy to overcome them. He raised $2,500, running from Welcome Bay to Mauao while wearing a weighted vest.

John Brown (far left), and Jack Te Moana (far right) shared their experiences battling bowel cancer with Head of the Movember charity Robert Dunne during the Mauri Ora event.
Attendees of GPNZ’s first hui for its Māori Health Leaders rōpū in 2022.
Māori health leaders unite in Tauranga Moana
Our PHO had the privilege of hosting the GPNZ Māori Health Leaders rōpū in February 2022. Established two years ago, the rōpū is a collective of Māori Health leaders from across the national PHO network. It is currently chaired by Irihāpeti Mahuika.
The group had a tough 2021 with many of the planned hui cancelled. This made the event in Tauranga Moana in February extra special for everyone.
Participants identified four key areas for development including Māori governance and partnership, recruitment of Māori into primary care, General Practice support tools to make Māori health planning intentional and authentic, and the development of Tikanga within our own whare (both GPNZ and PHO networks).
The rōpū then paved out a progressive workplan.
A wananga was held with specialist weaver Jenny Firmin at Hungahungatoroa Marae in Matapihi in July to take more people through the steps to weave a wahakura (safe bed) for pēpi.
Evolving quit smoking support for hapu māmā
A long-running wananga providing support for pregnant wahine Māori in the Western Bay of Plenty has been rebranded with new digital tools available to help them quit smoking. The Ūkaipō programme, funded by Te Whatu Ora, Hauora a Toi Bay of Plenty, has adopted the Heru & Hapū Māmā branding and digital resources following successful pilots in the Waikato and Eastern Bay of Plenty.
Delivered over six weeks, the local programme now combines three face-to-face sessions providing an opportunity for whānau to weave a wahakura (safe bed) for their baby. Participants also learn from health and social service providers with a take-home resource pack and digital app for participants to access in their own time.
In June a facilitation training workshop, led by programme developer and KaiRua founder Patrick Salmon, was held at Hungahungatoroa Marae in Matapihi for Western Bay of Plenty and Eastern Bay of Plenty providers to learn more about the online resources and how they can support wahine to become smokefree.
PHO health promotion coordinator Tiana Bennett says the transition from Ūkaipō to the Heru & Hapū Māmā programme reflects a need to engage with pregnant wahine Māori in new ways.
“The pilots have been really successful, so we wanted to bring Heru & Hapū Māmā across to the Western Bay,” she says.
“Patrick cleverly uses online learning and innovative augmented reality (AR) technology to connect with wahine and motivate them to make positive lifestyle changes for themselves and their whānau.”
Realising personal strengths
While there is a core focus on smoking cessation education, the KaiRua resources also empower hapu māmā to realise their personal strengths so they can have confidence to make changes for better maternal wellbeing.
In developing the kaupapa Māori programme, Patrick says the aim is to target wahine with education that supports their cultural identity of who they are, so they can achieve their goals.
“To build equity for positive Māori health outcomes and wellbeing, services must be culturally responsive and empowering. Heru & Hapū Māmā delivers tikanga and ancestral knowledge in a way that motivates participants to quit smoking.”
Online learning apps
Using the KaiRua app, wahine can access a three-part online series for education at home. Experts featured in the ‘digi-wā’ cover the philosophy of the heru, dealing with loss, grief and trauma, overcoming cravings with cooking, breathing and meditation techniques, reflective thinking, using kai to counter boredom or idle hands, and using karakia to meditate.
The online learning complements group sessions held at marae around the Western Bay, says Tiana.
“Similar to Ūkaipō, these sessions are a chance for wahine to connect with other hapu māmā, health and social service providers that work with whānau, and weave a beautiful wahakura that becomes a safe sleeping device for their pēpi.”
Three-way partnership takes on long-term conditions
A pilot programme that provided support to patients with long-term health conditions and their whānau will roll out across the Bay of Plenty thanks to further PHO funding.
Te Āhunga Whānau was piloted in the Western and Eastern Bay of Plenty over 12 months, operating in partnership between the PHO, Ngāti Ranginui Iwi in the West, and Tūhoe Hauora in the East. The whānau focussed model of care saw mobile nursing and kaiāwhina teams work with patients from five practices in the pilot stage.
An evaluation of the programme was carried out early in 2022, with feedback from participating practices helping to inform the next stage of development.
Team Lead Sarah Johnson says everyone was “fired up” to see the programme permanently adopted, involving three practices in the West (Katikati Medical Centre, Gate Pā Medical Centre and Ngāti Kahu Hauora), and The Doctors Total Health and Kopeopeo Health Centre in Whakatāne. Ngāti Ranginui Iwi and Ngāi Tūhoe Iwi in the Eastern Bay of Plenty are partnering with the PHO in the roll out by employing registered nurses and kaiāwhina to work with whānau referred to the programme by their GP.
“It’s a co-designed, whānau-centric, holistic model of care that we know can be life-changing for patients,” says Sarah.
“It’s not just focussed on responding to the long-term conditions of an individual, such as diabetes, asthma, or heart disease. It also supports people and their whānau to address the social issues that might be getting in the way of them having a healthier life that’s fulfilling for them.”
The first step for patients referred to Te Āhunga Whānau involves kaiāwhina building relationships with patients and their whānau. A holistic assessment will identify their individual wellbeing goals and any additional support the patient may need.
“For a lot of people who are struggling to stay on top of their health, there can be many other things that contribute to that,” explains Sarah.
Kaiāwhina can work with whānau on everything from working with Work and Income or the Ministry of Social Development, to looking at their tenancy agreements, housing issues, or helping them to put food on the table.
“It’s taking into account the social determinants of health, and the physical impacts they have on wellbeing. This also reflects Te Whare Tapa Whā, a Māori health model that explores the four cornerstones of hauora for Māori – taha tinana (physical health), taha wairua (spiritual health), taha whānau (family health), and taha hinengaro (mental health). In time, we expect more practices will see the value of this and be a part of Te Āhunga Whānau as well,” adds Sarah.
Whānau benefit from the programme for up to six months, allowing sufficient time to provide them with tools for effective self-management.
Equity Champions
Local practices gather for the inaugural Network Equity Champions rōpū
General practice staff from Tauranga and Whakatāne gathered for the inaugural Network Equity Champions rōpū in September to discuss health equity challenges and how to best overcome related issues.
Staff from various practices volunteered to form the ongoing discussion group, sharing experienced successes, challenges, tools, and programmes when it comes to health equity and serving marginalised communities.
The group was led by members of the Western Bay of Plenty Primary Health Organisation, including Director of Māori Health and Well-being Kiri Peita, Equity Programme Lead Michaela Kamo, and Iwi Network Services Lead Waimaria Awa, as well as the Network Services Team including Nick Page, Laura Penny, Donna Hardie, and Emma Skellern, who facilitated and encouraged the open discussion.
With the goal of helping General Practice staff overcome health equity barriers, the PHO team encouraged and facilitated participant-led discussions and feedback, drawing on lived experiences to gauge their wants and needs on their health equity journeys.
The ongoing rōpū will help the PHO assist practices in implementing the tools they need to reduce health barriers and serve marginalised community members.

Rōpū members put their heads together to highlight health equity challenges and goals.
Associate Health Minister Hon. Peeni Henare attended a function in Te Puke to learn more about the Mataora service in July. Pictured (left to right) Mataora Tamoko practitioner Karam Hood, Poutiri Trust CEO Kirsty Maxwell-Crawford, Awanui Mataora practitioner, Hon. Peeni Henare, Awanui Hauora GM Uta Roretana, Ngāti Ranginui CEO Mel Tata, Pou Tikanga Hori Ahomiro, Maara Kai Facilitator Paul Tuanau, and Poutiri Programme Manager Ray Wihapi.
Cultural and clinical therapy combine to restore health
A new collaborative kaupapa Māori mental health and addictions service operating in the Bay of Plenty is helping to restore whānau wellbeing by combining traditional cultural practices of healing with clinical therapy and education.
Whānau who access the Mataora service through a range of providers connect with clinical and cultural practitioners as part of a holistic approach that works to address the harm and associated behaviours caused by trauma.
At Poutiri Trust, whānau have access to healing via tā moko, while Ngāti Ranginui whānau have an opportunity to reconnect with their whakapapa using a ‘whakapapa navigator’ or esteemed genealogist. The therapies work alongside trauma counselling provided by clinical psychotherapists.
Following a successful bid for funding from the Ministry of Health, six Bay of Plenty providers are now offering the service: Poutiri Trust, Ngāti Ranginui Iwi, Te Ika Whenua (Murupara), Ngāti Kahu Hauora (Bethlehem), Te Awanui Hauora (Matakana Island) and Kimi Hauora (Tamapahore).
Poutiri Trust general manager Kirsty Maxwell-Crawford says the collaborative contract ensures that people in high needs areas, particularly Māori whānau, have better access to mental health and addiction services.
“Historically, access to services at a primary healthcare level have been poor, especially for Māori,” she says. “This contract addresses those unmet health needs, particularly for those most impacted by health inequities.
“This is a new approach but it also reflects the healing modalities of Te Ao Māori that have been very present in whānau, hapu and iwi for 23 generations. We’ve designed the service so that whānau are free to choose a range of clinical and cultural options in their wellness journey.”
Roy Nathan manages the Taiparirua team that delivers the Mataora service for Ngāti Ranginui Iwi on 9th Ave in Tauranga. He says the referral process recognises how “there’s more than one way to get into a whare.”
“We are a whānau-inclusive iwi with a range of services, so in working with whānau in one area, such as social services, we may identify someone who may also benefit from Mataora. Whānau can also self-refer, and choose the hauora provider that is closest to them, or one they have the strongest relationship with.”
While Ngāti Ranginui Iwi and other providers have operated other community mental health and addiction services before, this service stands out for its cultural component and its focus on trauma as a major driver of addiction and substance abuse, he says.
“Ninety percent of whānau with substance abuse have a history of trauma that’s led to unhealthy relationships and behaviours. But rather than focus on what they’re doing wrong, our service looks at what they’ve been exposed to in their hikoi through life.”
This year, Ministry funding has helped Ngāti Ranginui employ both an adult and child and adolescent trauma therapist, a genealogist and a non-clinical educator who visits businesses, organisations and schools to provide wellbeing education. The genealogist helps to restore lost connection for whānau.
“As Māori, we stand on the shoulders of those who have gone before us,” says Roy. “For whānau who present to our service in a state of negative noa, the navigator can help to restore mana and motivate them to transform by connecting people back through generations.”
New healthcare responses to family violence breaks taboos
A three-year research project aiming to strengthen primary healthcare approaches to family violence is reframing the way we talk about responses and developing a network of health and social care professionals dedicated to prevention.
The Atawhai project, funded by the Health Research Council of New Zealand through the centre of Interdisciplinary Trauma Research at Auckland University of Technology (AUT), is participant-led and involves working with primary care health and social workers to develop tools, resources, knowledge, and connections. The goal is to make it easier to respond to whānau impacted by family violence.
The Atawhai team has facilitated the research process by drawing on participant knowledge and experience, which has shaped discussions, findings, and solutions.
“We’ve had seven one-day deliberative dialogue workshops where participants have come together to identify system pathways and tools that professionals can use to make it easier for them to respond to family violence,” says Dr Claire Gear, Atawhai project lead.
“Frontline practitioners have shared their collective experience, wisdom, and uncertainties to build the confidence to have conversations with family violence victims, knowing they have support for their practice.”
A series of practice gems as well as four key pathways to responsiveness have been developed through the workshops, providing healthcare workers with useful resources.
“We challenge participants to look at what’s needed and work with them to develop what is missing.
“The network of peer support means practitioners can discuss ongoing care options with someone they trust. When you have more people involved in whānau care it takes an individual burden off the health professional,” Claire adds.
“It’s about recognising that kōrero about family violence can be many shared moments in time underpinned by tika, pono and aroha. We realise we don’t have to fix problems in that moment, but rather be someone that whānau can trust to walk alongside them.
“We’re developing supportive tools and resources to help practices share their experience of engaging with whānau and the challenges associated with that. There’s a lot of fear and uncertainty involved in family violence, so it’s about sharing that load with one another.”
A strong component of the project involves raising awareness of family violence as a key determinant of ill health at policy and practice levels, says Emma Skellern, participant in the Atawhai research project.
“The programme has been developed to empower participants to come up with the content and to advocate, step up and create change. It has created a network that healthcare workers can sign up to for peer support around these issues,” explains Emma.
Atawhai is founded on a Te Tiriti based partnership and has a strong Te Ao Māori presence. The project began in September 2020 and is due to finish in October 2023.
“This is when the funding finishes, not necessarily the work. It’s a rare opportunity to have a research project that spans over such a long period of time. It’s helped us form strong relationships which will continue beyond the project,” says Claire.
Moving forward, the project team is looking at leadership and sustainability for the long term by developing an investment plan to gain post research funding. Local and national representatives are also guiding a key knowledge translation strategy, mapping out how the knowledge generated can improve responsiveness to family violence.
As an extension of over a decade of work, the research team are additionally looking at ways to evidence the impact of the research, with sights set on conducting future research around how to optimise health and wellbeing when accessing family violence services.
“It’s been a big learning journey for everyone and has provided the time and space for participants to reflect and critique the way we think about practice,” says Claire.
“Healthcare has traditionally been outside of the typical family violence response, so we’re bringing health into the picture to understand the role we can play.”
Unique partnership to support gang whānau
Providing a unique model of care to support gang whānau and marginalised communities, the Western Bay of Plenty Primary Health Organisation (WBOPPHO) has partnered with Waiariki Whānau Mentoring Trust to assist the organisation to build and strengthen its hauora arm.
Waiariki Whānau Mentoring Trust is a Māori owned social and health service provider that offers brokering and advocacy services to support whānau in many aspects, including health and wellbeing. Building trusted relationships within the gang space, the Trust sits as a connection between marginalised communities and other service providers.
“We facilitate honest discussions about unresolved trauma and then lock in support, such as triage, housing options, mental health and drug addiction services, suicide prevention, weight loss advice and more,” says Waata Heathcote, Board Chair at Waiariki Whānau Mentoring Trust.
The organisation has a non-traditional approach to healthcare, improving health outcomes and saving lives by being responsive and flexible, identifying trends by meeting whānau in crisis, and working backwards.
“Waiariki came about because of the inadequacy of a system that is not conducive to the needs of marginalised communities. Our model sits outside current health and social frameworks because it’s been designed to catch people that fall through the gaps. It’s the net that serves those that the mainstream health system doesn’t serve.
“We are a whānau movement, not an organisation. We walk alongside whānau and our team has worked hard to build a high level of respect with rangatira within gangs by embracing passion, commitment, openness, and honesty to build relationships.
“Our diverse workforce uses their lived experiences to help our community members. We have just over 50 employees, nine or ten of which are patched gang members,” Waata explains.
At the beginning of 2022, the WBOPPHO formed a relationship with the Trust by committing to a five-month funding period to help build an outreach clinical, nurse and navigator team.
“I didn’t want to create a partnership with the PHO because a partnership is a business model,” says Waata. “What I was looking for was a relationship. I wanted to create connections with trusted people and organisations who can help us continue our work.”
Evolving overtime, the PHO is now focussed on providing clinical support and advice about what’s needed to establish a hauora arm.
“We just love being involved,” says Phil Back, General Manager of Network Services at WBOPPHO.
“There are a lot of opportunities that can come out of this partnership. If we are instrumental in making sure that Te Aka Whai Ora promotes the Trust through commissioning conversations with Te Whatu Ora, there is recognition, capacity, and ability to financially support them. That is, in itself, a benefit of the relationship.
“The beauty of what I embrace is that the Trust is out there doing the hard mahi and making a difference, but not in the way we traditionally measure outcomes because what they do is not traditional. Their model is built on relationships and trust, not partnerships. The intent is absolutely brilliant.”
It was during the COVID outbreak that the Trust was formed because opportunities were identified to work with marginalised communities. A clinical arm was formed to provide health and wellbeing connections with community members who weren’t part of the mainstream system.
“When COVID hit, we started to look at how we could reach marginalised communities in a medical capacity, enabling them to stay at home and survive for the 10-day COVID isolation period,” Waata says.
With the establishment of this new clinical arm, the Trust was able to form relationships with gang members and marginalised communities that would otherwise have missed out on services and help.
“During the Omicron surge, we got a call at 9.30pm reporting four or five potentially contaminated households. We deployed nurses out with RAT tests and had conversations with gang leaders in the community to find out what they needed from us,” explains Waata.
“We were able to do things that other providers couldn’t because we have solid, trustworthy relationships with these community members. Our teams were on the ground at 10pm on a Saturday in gang territory. The next morning by 10am we were back on the ground with RAT tests.”
As the first real experience for the newly established nursing team, the Trust was able to RAT test 93 gang whānau, discovering 21 positive cases, recalls Waata.
“We focused on whānau and got the job done. If it wasn’t for us being able to reach these communities, we were told that it would’ve been a challenge to suppress the Omicron strain.”
The Trust has also been able to further assist their communities post-COVID by offering a range of health services including screening and smear tests for wahine and tane, general health checks, vaccinations and immunisations, health promotions, and more.
With a health kaupapa, the Trust has a mobile nursing team that can visit whānau in their homes, as well as three nursing clinics.
“Most marginalised communities such as gangs, homeless, and those living on the fringe just want to connect with people who will listen. That’s exactly what we do, for the betterment of our people and the betterment of our whanau,” adds Waata.
The Trust additionally mentors whānau to connect with services independently.
“Access criteria currently block members of these communities, but it’s important to remember that behind a patch is a whānau member who needs a house or health check-up,” says Soifua Pearson, Te Wai Aio Team Lead.
“Equity comes from bringing whānau together and this can be done through the restoration of relationships and reconnecting with identity and whakapapa. We challenge them in a loving way.”
Our Programmes
Te Whatu Ora Funded Services
A comprehensive range of targeted services, including Community Radiology, focused on reducing Emergency Department presentations and hospital admissions through enhanced service delivery within a primary care setting and ensuring people remain connected to and cared for by their primary care provider.
This suite of services, provides free access for children under 14 years of age and subsidised access for High Need and Community Service Card holders. Services include extended hours offered through General Practice on weekdays and after hours on weekends, contracted after hours services through Accident and Healthcare and telephone-based access to health advice and triage.
A targeted approach, supporting General Practice teams and referred patients with a comprehensive range of medicine management and adherence, and specialised prescribing support and advice. This is delivered through Medwise. Additionally, supporting effective discharge, medicine reconciliation and care for residents within Aged Residential Care facilities through an ARC specific service framework.
This service provides for a range of therapeutic services such as a social worker, group therapy, GP or nurse extended consults, counselling or psychological support for depression, anxiety, Alcohol/drug issues and youth mental health. This support is delivered within a ‘Stepped Care’ model, by a range of contracted and internal specialist therapists. This service is one of the PHO’s busiest.
A service that provides intensive care to those managing opioid dependency. This service is delivered by an increasing number of GPs in partnership with the BOPDHB’s specialist Bay of Plenty Addiction Services.
Western Bay of Plenty Primary Health Organisation has taken the lead in the rollout of the nationally recognised Health Care Home Model of Care across participating practices within the BOP. This initiative is supported by a significant two-year investment through BOPDHB and additional investment of both funding and in-kind resource from both EBPHA and the PHO to support delivery over the next three years. The Health Care Home Team significantly contributed to the revised national model of care, which now has a stronger focus on health equity, consumer involvement and honouring Te Tiriti o Waitangi.
This service is for anyone who is enrolled in the general practice whose thoughts, feelings or actions are impacting on their health and wellbeing. This model of care is part of a suite of services being developed to expand access to, and choice of, Primary Mental Health and Addiction support. Health Improvement Practitioners (HIP) and Health Coaches (HC) work as a part of the practice team to provide brief intervention focused on strengthening self-management strategies. There are no barriers to accessing this support.
A devolved service from secondary care, focused on providing timely access to iron infusion, for a dedicated patient cohort, within a community setting thus, reducing demand on hospital services and minimising travel and access barriers for patients.
A targeted service delivered through General Practice to an eligible population with a focus on reducing unwanted and/or unplanned pregnancy.
This is the PHO’s most comprehensive integrated service, delivered through General Practice, community-based contracted providers and in-house Dietetic and Diabetes Specialist Nursing resources. It focusses on Cardio-vascular Risk Assessment, diabetes detection and management, high riskdiabetic foot podiatry services, retinal health, nurse specialists and self-management education. Pulmonary Rehabilitation also falls within this suite of services.
Under sub-contract to EBPHA, an Outreach Immunisation Service is provided to support General Practice maximise coverage of childhood immunisations across the rohe. The service has worked collaboratively with Support to Screening Services to pool resources and efforts, building and developing internal capability which in turn has increased immunisation outreach services capacity.
This is a package of care approach, supporting General Practices to manage wound management for post-operative patients discharged back to their GP.
The Bay of Plenty is included in statistics for the highest rates of skin cancer in the world. This service enables lesions to be surgically removed by approved specialist credentialed general practitioners. An independent specialist in skin cancer surgery is engaged to triage each referral, ensure clinical standards are maintained and the DHB-assigned resources used well. The PHO is also responsible for credentialing all approved clinicians.
Delivering a comprehensive range of primary healthcare services across secondary schools within the Western Bay of Plenty, this service offers both nurse-led services during the school weeks and GP clinics on a contracted basis. These services are underpinned by excellent partnerships between schools and the PHO and has reflected continued increases in access to services by the student population.
There are two areas of focus within this service. General Practice teams are enabled to offer support to patients who indicate they want to quit smoking. This is not dependent on a quit date being set and achieved. The other focus is a Heru and Hapu Mama wananga for pregnant wahine Māori, operating under the gifted name of Ūkaipō. Inclusive of the extended whānau, the service focusses on health lifestyle choices for both māmā and pēpi, including smoking cessation.
A nationally funded cervical and breast screening service focussed on improving screening coverage rates for priority women. A successful programme that creates opportunity for eligible priority population women: Māori, Pacific and Asian wahine to screen for breast and cervical screening. We give choices, we break down barriers, we kōrero with wahine, and we look after our communities. We create opportunities through a breast screen mobile clinic, community pop-up clinics, and support hauora events led by Iwi and Hāpu.
PHO Self-funded Services
Mau Rakau programme aims to train rangatahi māori in the art of mau rakau (traditional weaponry) through regular wānanga. The art form draws from a basis of training methods traditionally used by tupuna (ancestors). In a contemporary context the programme endorses discipline, culture and the importance of relationships and is underpinned by matauranga māori (knowledge) and primarily delivered in te reo māori.
A mobile primary healthcare and social work service delivered after hours across several high-need communities; this is a free walk-in service. The model of care incorporates health, social, welfare, housing and cultural wellbeing and needs through a whānau and community approach across all ages.
Operating as a mobile and adaptable resource, this highly regarded registered and specialist nursing service is focussed on support to our most vulnerable populations on behalf of our General Practice network and iwi partners through provision of community-based outreach nursing care.
These are a physical activity and healthy lifestyle-focussed suite of services, supporting individuals and their whānau who are seeking the benefits of improved levels of activity and improved lifestyle choices. Sport Bay of Plenty has been contracted to provide these services for more than 10 years.
Introduced in 2018 to support General Practice to engage with and support patients access and recover from the Hepatitis C infection as part of a national eradication program.
A limited resource intended to enable General Practice to provide more intense support during end-stage palliative care to the patient and their family through subsidisation of service costs.
(incl. System Level Measures, CVDRA and national health targets)
A range of financial incentives are available to our general practice network to recognise optimal clinical performance in several key areas including CVDRA, 65+ seasonal flu coverage, smoking brief advice, and breast and cervical screening coverage for Māori women. System Level Measures funding available through the Ministry of Health is supplemented by the PHO where national financial incentives no longer exist.
A dedicated funding line assigned to General Practice to use at their discretion, to assist high-need patients where financial barriers reduce access to health services. This has been particularly welcomed by practices wanting to support vulnerable population groups during and after the impact of COVID-19.
A limited level of funding provided directly to General Practices to subsidise the costs of diagnostic services for patients that do not meet the eligibility criteria for access to the Te Whatu Ora-funded Minor Skin Surgery Service.
Koiora is a leadership development programme that focusses on enhancement of hauora Māori for rangatahi. The programme provides for the transfer of traditional and cultural knowledge as a basis for encouraging mental and spiritual health, good nutrition, regular physical exercise and enriched cultural connectedness. It is a forum that provides mentoring, sharing of knowledge, networking, and goal setting.
The service includes a range of programmes aimed at assisting and empowering whānau to improve and develop their health and wellbeing journeys. The concept of Mauri Ora extends beyond physical healthcare to include factors such as spiritual wellness, mental health, and connectedness to their whānau and community.
The Kaupapa Māori Mental Health Service offers three programmes within this service: Mental Health and Addiction Co-Existing Problems Counselling, Trauma Counselling, and Peer Support Advocacy. The programme is culturally responsive to address Māori wellness needs, either individually or with whānau through various therapeutic approaches.
This service works with social housing tenants and provides co-ordination and advocacy services that aims to stabilise the home environment of Accessible Properties Limited (APL). The service delivery approach is a whānau support model that works alongside whānau to identify and manage health and wellbeing issues, with the view that by developing a relationship based on support and trust these issues will be able to be addressed.
The IGT programme supports GP teams to target patients with pre-diabetes who are at risk of developing diabetes and cardiovascular disease.
Funded appointment to support General Practice to undertake insulin starts independently.
A highly regarded service that focusses on the care of acute diabetics and consultative support to clinicians, operating as a component of the long term conditions suite of services through dedicated PHO funding.
A range of community-based clinics designed to improve accessibility to care and provide a range of services including health assessments, vaccinations, and smoking cessation advice.
The dietitian provides a range of services for our enrolled population over 18 years old within PHO-delivered services, including having a key role in the provision of self-management groups. One-on-one consults are also available.
WBOP PHO works closely with St John and ED to fund General Practice to manage eligible redirections from these services.
This pilot was initiated mid-2021 within both the Western and Eastern Bay of Plenty. This service enables a registered nurse and Kaiāwhina to work with a dedicated neighbourhood of General Practice enrolled populations to provide mobile outreach services to those most at risk on behalf of their practice of enrolment.
The PHO coordinates and delivers a comprehensive medical and nursing continuing education service across our provider network, which is available both face-to-face and via Zoom. Evening sessions are delivered to increase accessibility and the PHO also supports a range of day time workshops for the management of long-term conditions. WBOPPHO is also part of a collaboration between the midland region’s five DHBs and eight PHOs to offer the Midland Collaborative Recertification Programme for Registered Nurse Prescribers in Community Hhealth.
In Focus
COVID-19 Round Up
How COVID-19 united us
When the Delta variant arrived in the community at the end of 2021, and then Omicron at the start of this year, the PHO’s COVID Primary Response Team showed the value of collaboration across providers to care for people in the community as they recovered at home.
The unpredictability of working in health during a global pandemic has given rise to some positive consequences, particularly in the realm of heightened collaboration and support for each other, as well as reaching marginalised members of our community who weren’t connected to a GP prior to COVID-19.
Super Saturday and milestones
General Practice Teams across the Western Bay pulled out all the stops to get behind Super Saturday on 16 October 2021. Eleven of the PHO’s practices participated in the national vaccination event.
The Bay of Plenty district reached its 90 percent first dose COVID-19 vaccination target on 30 November 2021. By that date more than 194,000 people in the region had received their first dose. More than 80 percent of the district’s residents had been fully vaccinated. Within the Pasifika community, more that 95 percent had received both doses. On 4 January 2022 90 percent of the population were fully vaccinated.
Positive vibe at iwi-led max vax event
A ‘mass vaccination’ event led by Ngāti Ranginui has created a blueprint for further collaborative events involving kaupapa Māori health providers.
Ngāti Ranginui Iwi Society organised the Te Kupenga Hao drive-through vaccination event at Sulphur Point Marine Park on December 5. On the day Ngāti Ranginui iwi were joined by Poutiri Trust, Te Manu Toroa, and Te Pare ō Toi nurses from the Bay of Plenty District Health Board’s outreach team.
Collectively, they vaccinated a total of 170 people throughout the day – 90 per cent of them Māori. About one-third were first doses. Chief executive Mel Tata says there were more than 100 participants in the first hour of opening.
“It was quite a complex operation that was bumper to bumper at first, but we managed well because we had a great site plan that handled the pressure in that first hour of entry.”
On the day, there were spot prizes, icecreams, and kaimoana vouchers. The fisheries entity belonging to Ngāti Ranginui made vouchers available through its distributor Takitimu Seafoods in support of the vaccination kaupapa, says Mel.
“As an iwi we have the ability to draw on all our resources, including our kaimahi working in health, to create opportunities for our whānau to make the choice to get vaccinated.
“It was a great example of kotahitanga with everyone coming together with a common goal. We have this event as an example of what can be achieved when we all work together.”

The CPRT team, led by Sarah Johnson (centre), and administrators Renee Still (left) and Jen Moore (right) have developed local COVID referral processes.
Reaching the unenrolled population
COVID data revealed that 10 percent of patients testing positive for the virus each day in the Bay of Plenty were not enrolled with a GP. The observation followed analysis of local COVID data by Network Services Development Advisor Trish Anderson and the COVID Primary Response Team (CPRT).
The team was set up in December ahead of the Omicron response. Team Lead Sarah Johnson said, after a busy four months supporting the GP network to manage COVID positive referrals, the PHO was pulling together valuable population data.
An average of 1200 patients recorded positive RAT results each day in the Bay of Plenty earlier this year. About 10 percent are not enrolled with a general practice.
“These are the patients whom we know have largely been disconnected from health services for a while. In the future, we really want to reach out and support them,” explains Sarah.
“Even though we don’t know them as our patients, we have a duty of care and a sense of responsibility to ensure they have access to healthcare, should they need it.”
Sarah says many learnings have come from Aotearoa’s COVID response, which has brought into focus where some of the greatest community needs are.
Two administrators joined the CPRT team this year – Jen Moore and Renee Still. With Sarah, they’ve developed local COVID referral processes, working across the Bay of Plenty network and with telehealth providers Tunstall and Evolve.
Having operated through the peak of Omicron, Sarah says responding to COVID is like a spiderweb. “It’s intricate and sometimes we can get tangled up and trapped in the web! But we’re all connected and it’s quite beautiful when it all comes together.”
Practice perspectives
Western Bay of Plenty practice managers say managing COVID positive patients and the challenges of Omicron united their teams. The Doctors Tauranga, Epic Health, Dee Street Medical Centre and Fifth Avenue Family Practice volunteered to be part of the weekday roster, taking on responsibility for COVID patients who aren’t enrolled with a local practice.
Pam van der Nest from The Doctors Tauranga says they had a designated doctor who worked with the team on all COVID-positive patients. The workload was a ‘dramatic increase’ but working as a tight unit ensured they had the resources to cope. Working through the peak of a pandemic required everyone to ‘think on their feet’, she says.
“Volunteering for the roster was a chance to support our community…no amount of planning would have made it easier.”
At Epic Health, staff held short meetings, quickly determining those patients most in need. Working as a team and prioritising staff welfare was essential, says Practice Manager Wendy Sharplin. “Many hands make light work but we all needed to take a breath, and look after each other to make sure no one had overcommitted.”
At Dee Street Medical Centre, practice manager Camilla Wilkin says communication and teamwork were essential in managing COVID cases. “Patients we managed were hard to engage with and to contact. For the clinicians, it was a matter of allocating and directing the flow of patients, communicating, and pitching in.”
The team at Fifth Avenue Family Practice managed one of the earliest casual community cases at Mount Maunganui. Lessons learned through the process were later shared as a team, says practice manager Leigh Kennedy.
“We treated people who haven’t accessed the health system for years. Some asked us later to look after them and their whānau on a more regular basis, so that’s been rewarding.”
The experience also revealed some high welfare needs in the community explains Leigh, “It was a good experience to support those most in need. Being on the roster positioned us well to cope with the next phase that hit from January onwards. That’s when we started to see more of our own patients and all doctors shared in managing their care. Since we had the knowledge and systems in place case management was much more seamless.”
Practices rally together to get through winter months
Significant winter illness and unplanned staff absences, coupled with the lingering impact from COVID-19 and continued management of patient population’s broader health needs, has seen General Practices go to extra lengths this year to get through the harsh winter months. Collaborating, partnering, and buddying up with other local practices has become more common to help service increased patient numbers.
Working together, General Practices have called on their established relationships across the network, even mobilising a buddy system in some cases to help meet increased demand from patient populations, especially when challenged through unplanned staff shortages due to illness.
“Every practice has felt the pressure and they have been able to keep their doors open and see critical patients by supporting each other wherever possible through this season,” says Nick Page, Network Services Liaison at WBOPPHO.
Despite being two years on from the start of the pandemic and over its peak, this winter season saw high patient numbers with COVID-19 still circulating in the community, on top of the flu, colds, and other illnesses that New Zealanders have been exposed to with the reopening of our borders.
Donna Hardie, Network Services Liaison at the WBOPPHO, says that practices have juggled things around and utilised lessons that the COVID surge showed them, using an amalgamation of tools to help get them through the colder months.
“Staff have just got on with things. They have dealt with it as best they could, using a suite of tools such as deferrals, rebooking, shifting appointments, telehealth, and virtual screening. Triage has been important and some things they have been able to resolve over the phone.
“The COVID response and telehealth has meant that the surge has been dealt with better than it could have or would have been a few years ago. Over the phone services are truly embedded in what practices do now and are more accepted from patients,” Donna says.
Practices have additionally implemented advanced infection control processes.
“We have seen practices implement different infection control processes depending on what works for them. It has helped them keep patients safe from all respiratory illnesses in a way that hasn’t been done before,” Nick adds.
In Focus
Mental Health

Kate Vaaulu, a school nurse at Ōtūmoetai College, is helping to screen all Year 9 students using the YouthCHAT digital portal.
School nurse pioneers rollout of new mental health tool
Students starting Year 9 at Ōtūmoetai College will benefit from more targeted health and counselling services this year thanks to an online survey designed to pick up the most at-risk students earlier.
School nurse Kate Vaaulu is supporting the school to survey students via the YouthCHAT portal, a health screening digital tool designed by medical researchers at the University of Auckland. About 470 students are expected to complete the health survey before the end of Term 1. It will be the first time an entire cohort of students will be surveyed via YouthCHAT in the Bay of Plenty.
A previous attempt at Ōtūmoetai College was thwarted due to disruption caused by the first COVID lockdown in 2020. An earlier trial carried out in 2019 involving a smaller group of students demonstrated a number who required support for depression, anxiety, or self-harm.
Following that survey, the PHO allocated extra funding for a school counsellor to work one day a week. Students ‘red-flagged’ after completing the survey are seen by a counsellor that same day.
Kate says students will be set up to complete the survey securely and confidentially in the school’s IT room. The survey’s findings will help the school’s Wellness Team, including its two nurses, two doctors, four counsellors, physio and two first aiders, quickly identify students who need help.
“We already know we have students coming through from intermediate with issues stemming from trauma in childhood. The survey helps us to get support in place for them earlier in the year.”
Students needing mental health support will be directed to counsellors. Kate and her colleague Annalise Thomas will provide support to students with other issues, such as vaping, smoking, drugs, and eating disorders.
“We have a lot of hope for what YouthCHAT can help us achieve for students.”
This year Kate will juggle her YouthCHAT work with other school clinic responsibilities, including contraception and sexual health support for students. In 2021, she became the PHO’s first school nurse to become a Jadelle practitioner, which allows her to offer and insert long-acting contraception to young women at school. Last year she completed 26 contraceptive implants.

Bharat Mahajan, a program manager for the PHO and Mr Gay NZ for 2021, says the new service will improve support for all patients, including rainbow youth.
Removing barriers to mental health services
Bharat Mahajan is leading the PHO’s rollout of a new primary healthcare model that aims to better support patients with mental health issues and addictions.
The Integrated Primary Mental Health and Addictions (IPMHA) service is still in its infancy locally, with the Bay of Plenty DHB among the last five of 20 DHBs to implement the programme. However, Bharat’s experience at rolling out the Waikato’s IPMHA service helped to drive efficiency as the model becomes embedded within local practices. He is now a Health Improvement Practitioner (HIP) with the PHO.
“The benefit in rolling out a programme like this later is that we have the opportunity to learn from the experiences or challenges that other regions have faced.”
The service is already operating at Pāpāmoa Pines Medical Centre and Chadwick Health Care at all four of its local sites. It was developed by the Ministry of Health in response to He Ara Oranga, the Report of the Government Inquiry into Mental Health and Addiction. The Government allocated $455 million in its 2019 Budget over four years to expand primary mental health and addiction services nationally, enabling people with mild to moderate needs to access free and immediate mental wellbeing advice and support, when and where they need it.
No longer do patients need to meet specific criteria to access support – services are available for anyone whose thoughts, feelings or actions are impacting their health and wellbeing.
The service aims to reduce barriers to treatment by reducing waiting times for care, and ensuring the patient faces no additional costs. Under the IPMHA service, HIPs and Health Coaches work as part of the general practice team to provide patients with immediate support and tools for wellbeing.
The programme builds on the mental health and addiction expertise that already sits within practices, and strengthens collaboration between those practices, community health providers and DHB-led secondary mental health and addiction services.
Bharat, a former nurse, says the IPMHA service is innovative, and is focussed on delivering greater support to Māori, high health needs, youth, and rainbow populations.
“Support often starts with primary health. Most of us go to GPs as a first point of contact, so if we provide greater support there, we can minimise the risk of issues becoming much bigger or turning into a crisis.”
He says the demand for mental health support and addiction services had increased since the start of the COVID pandemic.
“We’re seeing a lot more rereferrals, and increased demand for child and youth referrals. That can come from extra anxiety and other complications at home. We know the rainbow community, and the transgender community, can experience a great deal of social isolation, which impacts their mental health.”
HIPs have a clinical role and are often qualified nurses, occupational therapists, and counsellors. They work with patients to encourage behaviour and lifestyle changes through primary health interventions, such as cognitive behaviour therapy (CBT) and focused acceptance commitment therapy (FACT).
Practices with 10,000 enrolled patients qualify for full-time practitioner support for five days per week. Health Coaches have a non-clinical role, using their life experiences to provide support. They can provide transport for patients and are more mobile to remove any barriers to access the service, resulting in increased access to health services, which addresses inequity.
“If a young Mum, for example, is stressed with a new baby, a Health Coach can visit them at a time and place that best suits them,” says Bharat.

Health coaches Liz Kriel and Natasha Edhouse actively support whai ora in the community, where and when they need it.
The bigger picture: Cheerleaders we all need are redefining primary care
They might not come with pom poms, but Health Improvement Practitioners (HIPs) are the cheerleaders we all need in our lives and are paving the way forward in modern primary healthcare approaches.
Natasha Edhouse and Liz Kriel are among eight Health Coaches or HIPs working across the Western Bay of Plenty and Whakatāne as part of the PHO’s Integrated Primary Mental Health and Addiction (IPMHA) services team.
The free service provides enrolled patients or whai ora with support in a timely manner to help guide them towards improved mental health and wellbeing. Common health barriers are removed by HIPs working alongside GPs and nurses to provide behavioural interventions and appointments are available on the same day.
Reducing barriers, such as transport, time and cost, are fundamental to helping people access the care they need in a timely way, says Natasha. HIPs’ non-clinical roles are mobile, enabling them to provide support where and when patients need it.
“We visit them at home or meet at a café or go for a walk up the Pāpāmoa Hills – whatever works best for whai ora. Not all our sessions are face to face; we can talk on the phone or on Zoom.
“A lot of people also work during the day so we can talk to a truckie on the phone hands-free in his cab when he’s driving to Matamata for an hour about his dietary needs. That fits into his day and it means he doesn’t need to park his truck for an hour to talk to us.”
In 2019, the Government allocated $445 million to expand primary mental health and addiction services nationally. Complementing existing primary health services, Natasha says health coaches provide whai ora with extra motivation and encouragement in relaxed settings to manage their health and wellness.
“Whai ora create their own goals and we’re like their cheerleader on the sideline. We’re not running the race but we’re cheering them on.”
Not all support relates to mental health, with whai ora also benefiting from discussions relating to lifestyle management, sleep hygiene, weight loss and long-term conditions, such as diabetes, asthma and gout.
Liz joined the team in April and says whai ora valued the support to get their health back on track.
“When we take people out of a clinical setting and we’re just walking and talking, people feel more relaxed and the conversation often just flows. We’re actively listening, providing empathy and compassion. There’s no judgement; we’re there to establish a relationship, respond to their needs and keep the kōrero going.”
If there is a need to connect whai ora with more clinical support, health coaches can make those introductions.
“We’ve got great relationships with Diabetes Tauranga, Sport Bay of Plenty and other community organisations, so we can make referrals if that’s what our whai ora need to get on top of their health,” says Liz.
Our Team
Our organisation is built on a foundation of hardworking professionals who look to the future and work together to achieve common goals.
Supporting the delivery of primary healthcare services in General Practices and across our provider network, our team doesn’t simply look to provide a helping hand, but to transform healthcare, bridge inequities, and keep our communities well. With strong leadership, our team is united in their mahi to cement our organisation as a national leader in eliminating health inequities for Māori.
Based on the challenges and opportunities of the Health & Disability reforms, we have created a new internal structure built on developing the right functional model to support us to deliver our business strategy and better health outcomes for Tangata whenua/people of the Bay of Plenty. This strategic repositioning will allow us to continue to manage and deliver contracts and services over the next two years and respond with a new functional group to assess needs, carry out research and development, and advance integrated care initiatives with a key focus on addressing inequity. Our ability to be agile and work in new ways underpins our success as we go forward in a changing sector.
As our team is our whānau, our new structure has considered staff feedback and hui over the last eighteen months, allowing us to focus on our strategy and purpose with the involvement of our entire organisation. With exciting new roles that will make a real difference to the community, meet some of the new PHO whānau below.

The PHO welcomed new whānau recently, including Health Data Analyst Guru Muthu, and Digital Systems Coordinator Hardik Chadha.






The PHO positioning to make the most of opportunities within the changing health landscape with new appointments
New recruits to the PHO this year added to the team by helping to strengthen our connections with iwi, grow workforce capabilities, and harness the power of data to deliver more targeted clinical services.

Matthew Davies, Waimaria Awa and Dorlé Van Der Westhuizen are among the PHO’s latest recruits.
Matthew Davies
Matthew Davies is our new Population Health Data Specialist, he provides strategic, technical, and analytical advice to support how the PHO develops and delivers data-driven health insights and analysis.
“I’m working with data users to enhance the data reporting that we currently have and to develop a strategy and framework for growing the role and quality of the insights we can use to improve our service, and how we can share data with our partners and stakeholders to help them do the same,” he says.
Dorlé Van Der Westhuizen
New Workforce Development Advisor Dorlé Van Der Westhuizen is excited about the projects ahead of her, and the PHO’s growing team. One of her immediate tasks is developing a Workforce Development Strategy that aligns workforce development activities with the PHO’s strategic goals.
“This will provide us with a systematic approach to workforce development and ensure that we grow and develop our workforce in line with the strategic goals of the PHO and provide professional development opportunities to our provider network. The implementation of a new Human Resources Information System will also enable us to have detailed electronic employee and training records.”
Waimaria Awa
New Iwi Network Lead, Waimaria Awa, is responsible for providing advice, support, and services to ensure better outcomes for whānau, through working collaboratively with iwi networks, and more broadly across the PHO teams, with a focus on high needs populations.
“I am truly humbled to be working in this space and I am excited to be a part of the mahi and projects in the PHO moving forward. Poipoia te kakano kia puawai, nurture the seed and it will blossom.”
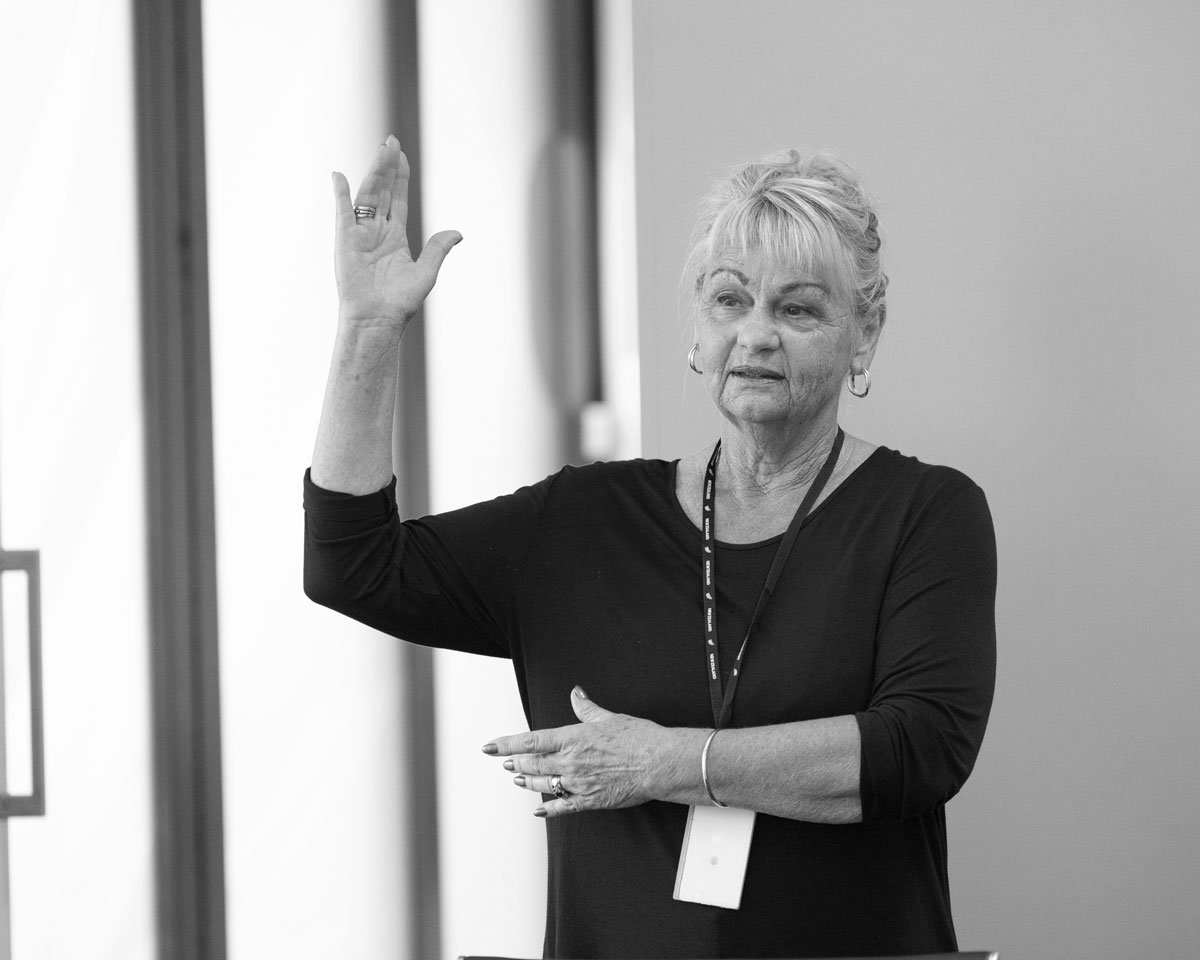
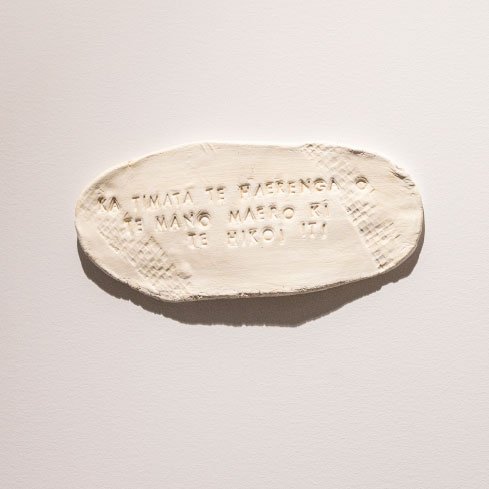
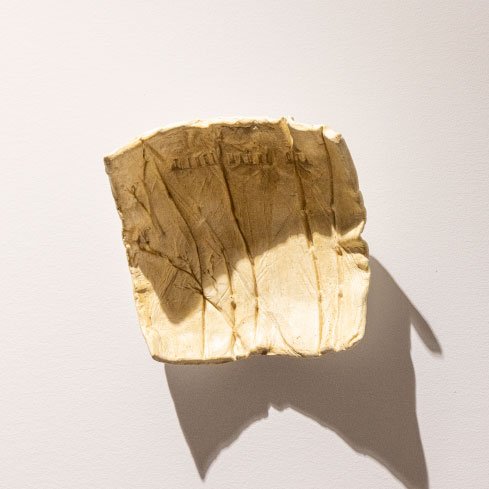
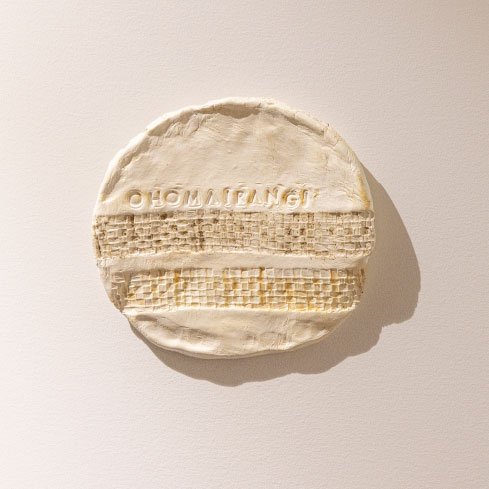
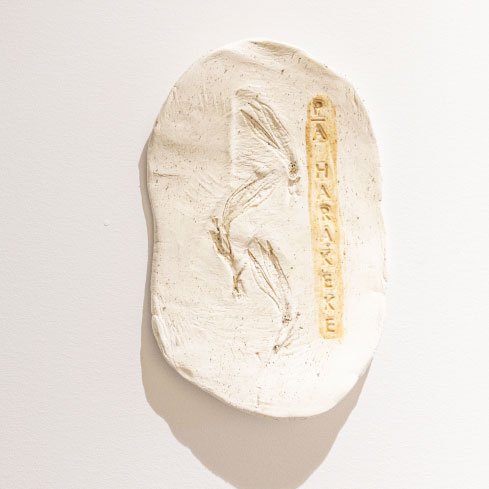
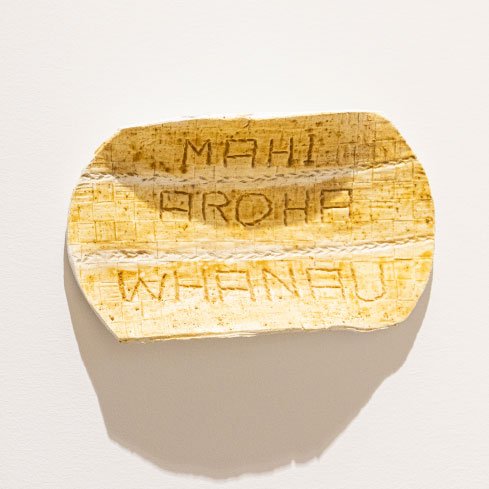
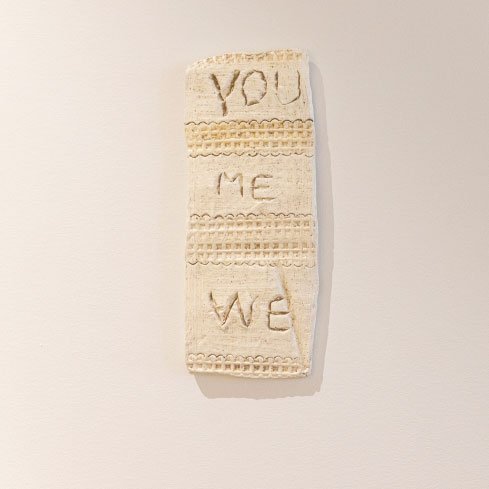
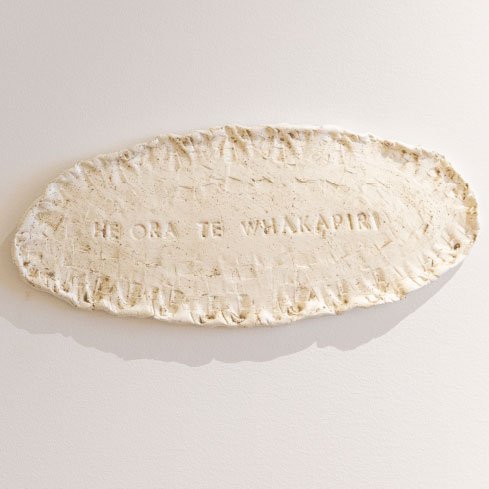
Our mahi toi that celebrates diversity and teamwork
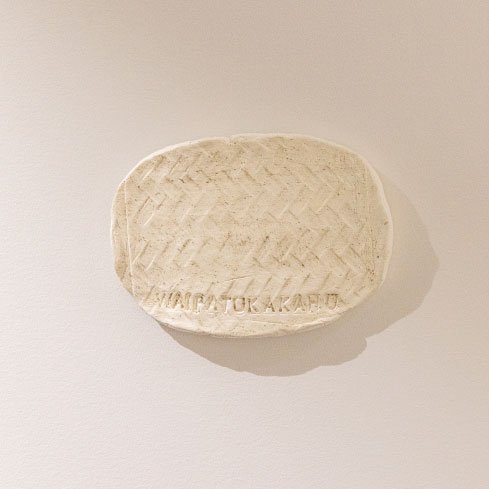
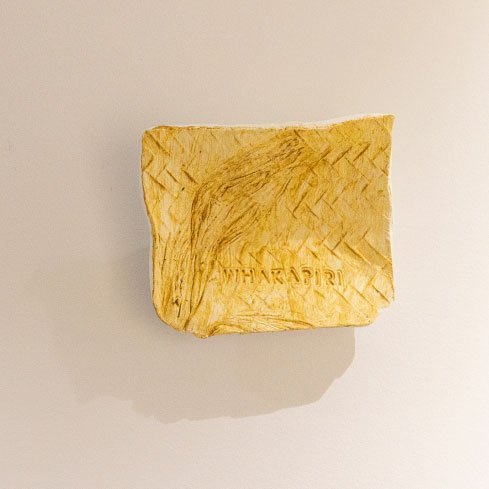
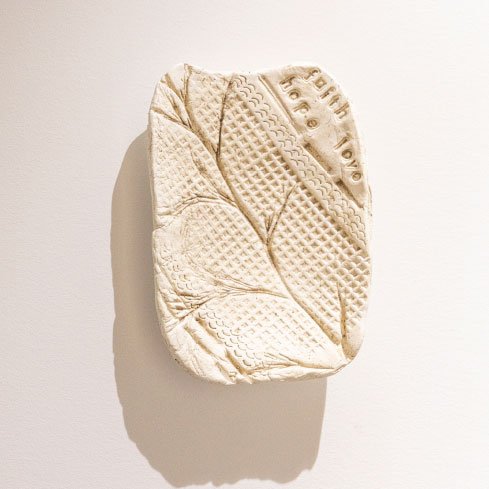
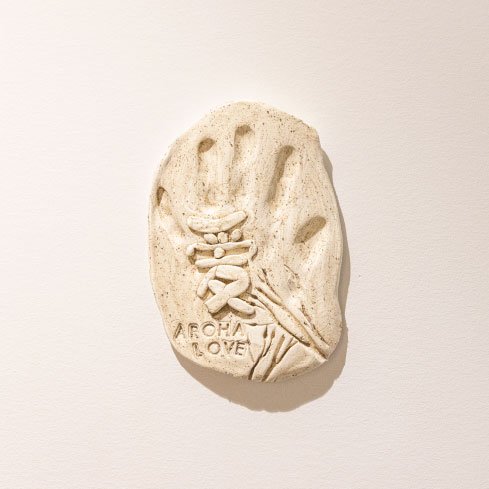
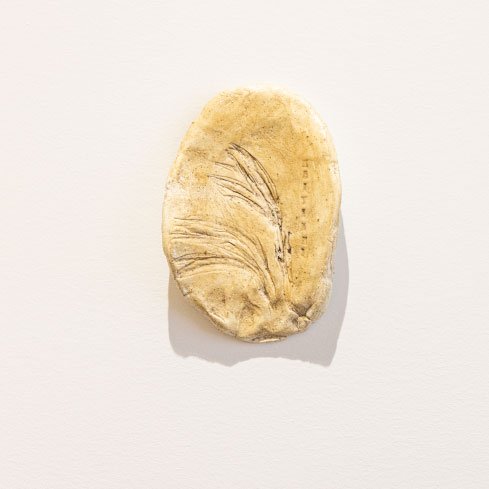
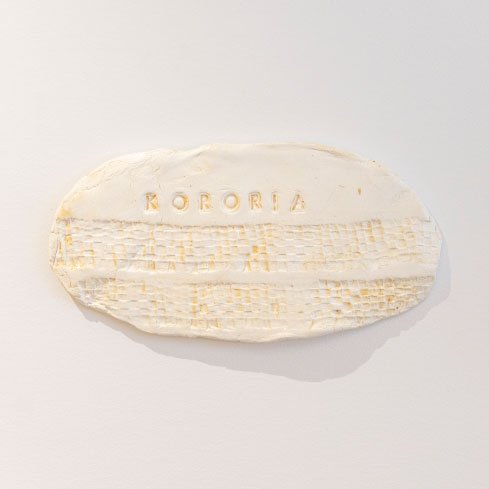
Taking pride of place on the wall in our First Avenue office is a collective installation of clay wall hangings created by the staff of the PHO.
The mahi toi (artwork) serves not only as a visual representation of the whakataukī, but as a celebration of diversity and the strength that comes from the group as we collectively rise to the challenge of reorganising our healthcare model to embrace a pro-equity approach and deliver improved services based on the needs and priorities of our local communities.
Created in a workshop facilitated by respected artist and teacher Maraea Timutimu (Ngāi Te Rangi, Ngāti Ranginui, Ngāi Tūhoe), participants used a combination of harakeke fibres, seeds and raranga (weaving impression) to create personalised clay wall hangings.











Bay of Plenty practice staff bond with local service providers.
Spirit of collaboration celebrated at expo
The WBOPPHO has taken every opportunity to grow the new ideas and relationships that have emerged over the last 12 months, and to strengthen the network.
One such opportunity, while emerging from the winter peak, was on Wednesday 21 September, through facilitating and hosting a Service Forum Expo. Inviting 14 local services from around the Bay to gather and connect with medical practices, the Service Expo provided healthcare workers with a unique opportunity to reconnect, create new collegial relationships, learn, grow, and develop post-COVID.
“The service landscape changes quite quickly and some of the services are new to the Bay of Plenty, so, this was a great chance for us to showcase the services and help local health and wellbeing workers connect,” says Emma Skellern, Network Services Liaison at WBOPPHO.
With food, drinks, spot prizes, draws and more, over 100 practice staff attended the event, displaying the close relationships between healthcare services across the Bay of Plenty.

He Pounamu sessions are interactive and available to PHO whānau either in the office or working from home.
More than language: our te reo Māori journey
Our PHO’s te reo Māori journey continues in earnest, with a dedicated Kaiako (tutor) working with staff one on one to provide more tailored support and encouragement.
This year Te Haana Jacob started working with staff who take part in fortnightly He Pounamu sessions to upskill in te reo Māori as part of ongoing professional development. Participation is voluntary and sessions are recorded so staff can refer to them later. Topics covered include pronunciation, mihi (greetings), waiata and karakia. Te Haana learned te reo Māori as a first language and enjoys sharing her knowledge with Māori and non-Māori, encouraging everyone to give the language a go.
“All you can do is start and try,” she says. “Hesitancy culls opportunity for growth… there is nothing wrong with trying and re-evaluating.”
In her sessions, Te Haana offers a variety of ways to learn and says everyone on a te reo Māori journey is “always a student, never a master.”
“All our strengths matter, and no matter how different we are, we can all collaborate and contribute to develop a strong team.”
He Pounamu started in 2020 following a staff survey, and is part of the PHO’s wider cultural journey, recognising the inseparable links between Māori language and culture. PHO director of Māori Health and Wellbeing, Kiri Peita, says it has been rewarding to see participants actively complete their ‘homework’ and engage with sessions.
“It shows a commitment to the journey, which recognises that whatever we learn, no matter how small, it is valuable and adds to our kete of knowledge.”
New clinical advisors
The PHO welcomed new clinical advisors Dr James Peckett, a GP at Mount Medical Centre, and Michelle Meyer, a nurse practitioner from Tara Road Medical Centre. James says working in healthcare during a global pandemic proved how agile General Practice teams could be.
“I think General Practices are now better at responding to change. A positive has been the enhancement to teamwork that only a liminal experience like a pandemic can develop.”
James expects that the upcoming health reforms will requires General Practices to be light-footed again, as they navigate how to incorporate business as usual into a new model for delivering primary care.
“Our agility thought COVID has us well-placed to respond to this challenge.”
Before working at Tara Road Medical Centre, Michelle worked to implement the Health Care Homes model at another practice and delivered services to a high needs population.
“This position [as clinical advisor to the WBOPPHO] allows me to not only use my nursing and nurse practitioner experience, but years of working in collaboration and partnership with GPs and practice teams, encouraging teamwork, quality improvement, and equitable services to meet the needs of the population,” says Michelle.

Our team donned pink in all its fabulous shades for Pink Shirt Day.
United in pink
On Friday 20 May our PHO staff stood together in support of Pink Shirt Day. The Mental Health Foundation of New Zealand’s annual initiative to fundraise and promote positive messages to reduce bullying. Pink Shirt Day has been celebrated since 2007 and is about people working together to stop bullying by celebrating diversity and promoting kindness and inclusiveness.
For our PHO whānau, it’s about creating a community where all people feel safe, valued and respected, regardless of gender identity, sexual orientation, age, ability, religion or cultural background. Kōrero Mai, Kōrero Atu, Mauri Tū, Mauri Ora – Speak Up, Stand Together, Stop Bullying!
Health & Safety
We’re committed to creating a nurturing environment for all our team and those who visit us. A place where people feel a sense of belonging and purpose, a place where mental and physical wellbeing are the priority, a place that is safe and positive. He tangata, he tangata, he tangata – it’s all about the people, the people, the people.
It is our core belief that all staff and associates of Western Bay of Plenty Primary Health Organisation, regardless of position, have the right and expectation to be able to work in, and visit, our organisation without fear of discrimination, bullying or harassment. Associates in this context may include contractors, visitors, committee members and governing board members. Our staff have developed an anti-bullying, anti-harassment and mana enhancing policy and staffroom poster. Also, our staff, managers and senior leaders have worked together to create a document that incorporates our shared values of inclusiveness (Whanaungatanga), empowerment (Mana Motuhake), achieving equity (Whai Mana), and showing respect for each other (Mana Motuhake). The document outlines that staff have the right to expect the following:
- They will be treated with kindness, professionalism and respect
- Their differences will be accepted and celebrated
- Less-than-optimal performance will be addressed respectfully
- Bullying behaviour will not be tolerated at any level of the organisation
Staff new to management roles will be given leadership training to guide them in achieving high outputs from their staff while maintaining professional and appropriate behaviours.
Our Health and Safety Committee includes staff and management who work together to share responsibility for instigating, developing and actioning measures designed to safeguard the health and safety of our employees.
As part of our health and safety responsibilities we have health and safety representatives who attend monthly Health and Safety Committee meetings, fire wardens who carry out bi-annual fire drills, and certified first aid officers at both of our sites – First Avenue and Whakatāne.
All new employees receive a health and safety induction and a workstation assessment.
All staff are involved in the annual national ShakeOut, which reminds people of the action to take during an earthquake – Drop, Cover and Hold.
COVID-19 restrictions mean that staff are required to wear face masks in the areas where they will come into contact with visitors, such as the hallways and reception. Surfaces are sanitised, and staff are constantly reminded to exercise good hand washing hygiene and stay home if unwell.

Hunting for clues during the Christmas party scavenger hunt at Memorial Park.
A time to celebrate
We kicked off 2022 with some whakawhanaungatanga (the process of establishing relationships) at a staff BBQ brunch on January 17. It was a great way to reconnect as a team, meet new colleagues, and energise ourselves for the mahi ahead.
This followed festivities celebrating Christmas and the company of whānau in December. 2021 was another demanding year for everyone involved in primary care, so it was a pleasure to take some time away from the coalface and enjoy some hospitality during a gorgeous evening in Tauranga Moana.

PHO team members celebrated Diabetes Action Month by participating in Sneaker Day.
Stepping up for diabetes
Team members wore their sneakers to work on 19 November 2021 in support of the first ever Sneaker Friday, a nationwide event encouraging New Zealanders to ‘step up’ for diabetes.
As well as doubling as a fundraiser, Sneaker Friday was one of many activities held during Diabetes Action Month to raise awareness and bring people together to take action over what has become New Zealand’s largest and fastest growing condition.
Diabetes nurse educator Brenda Newman says the PHO’s diabetes team was actively involved in events throughout November, with a focus on education in primary care.
A Diabetes Fundamentals Day was held for nursing staff who are either new to primary care or needed upskilling in supporting their patients diagnosed with diabetes to manage their condition.
“We covered information addressing inequities in care for Māori and Pasifika patients, the new diabetes guidelines, lifestyle changes relating to exercise and diet, and tips for how to run a nurse-led clinic,” said Brenda.
Guest speakers included a clinical pharmacist from Medwise and a podiatrist from Foot Mechanics.
The team also held an insulin start day for practices whose nursing staff needed upskilling on how to do insulin starts for patients.

New PHO value reflects passion for work
Following consultation with staff and stakeholders earlier this year, the WBOPPHO has formerly adopted a fifth value. We have added ‘Whai Ihi’ to reflect the value we see in expressing passion pertaining to our knowledge and expertise as practitioners working in primary healthcare. Showing ihi, joy, and excitement in our mahi helps us all deliver the best care in our community.
Our values
Collectively, these core value guide us on our mission to ensure positive and fair health experiences for all, so everyone can flourish.
Whanaungatanga
Inclusiveness and a sense of belonging.
Manaakitanga
Caring and showing respect for each other.
Mana Motuhake
Enabling people to be in control of their own health and wellbeing.
Whai Ihi
Expressing passion pertaining to our knowledge and expertise.

Decorated polystyrene balls, multimedia presentations and Matariki-inspired narratives demonstrated the many creative hidden talents of our PHO whānau at a team building event in June. Pictured here, Phil Back, member of Team Fu-Fu and the Fun Guys, proudly holds the team ball “Fu-Fu the Fun Guy”.
Ngā mihi o Matariki, te tau hou Māori!
For the first time in Aotearoa, Matariki was celebrated as a public holiday on 24 June 2022.
In the spirit of new beginnings, our PHO marked Matariki by making a $500 donation to Trees That Count, an organisation supported by Project Crimson, for the planting of 50 natives trees in Tauranga Moana.
MEN’S HEALTH
The Men’s Health Group tackled the Mauao base track. Pictured (from left) Laeton Packer, Phil Back, Dr James Peckett, Chris Dever, Nick Page (seated) and Ngāi Te Rangi chairman Charlie Tawhiao.
Small steps, big gains for tāne
Our PHO is ‘walking the talk’ by forming a new health group devoted to improving men’s health. The Men’s Health Group, made up of staff, iwi partners and Friends of the PHO, kickstarted activities with a walk around Mauao followed by coffee at a local café in May this year.The event coincided with Men’s Health Week and is the first of what is likely to be monthly activities aimed at making it easier for men to have conversations about their health and wellness. Group facilitator and PHO chief financial officer Laeton Packer says the casual get-togethers will be a chance for participants to open up in spaces where they feel comfortable.
“We know that men don’t tend to proactively talk to each other about their health but are more likely to in an environment where they are comfortable, such as at a BBQ, over coffee or during a physical activity.
“While we’re not directly targeting specific cohorts of men in the Bay of Plenty with our health messaging just yet, we do have the ability to walk the talk. The journey to better health needs to start somewhere and, as men within the PHO, we can actively role model.”
This year’s Men’s Health Week highlighted some alarming statistics for Kiwi men. A boy born today will live nearly four years less than a girl born in the room next door. He will be over 20 per cent more likely to die of a heart attack than a girl, and almost 30 per cent more likely to get diabetes. Worse, he is three times more likely to die by suicide or in a motor car crash.
Māori and Pasifika men live significantly shorter lives on average than men from other ethnic groups in Aotearoa. Soberingly, almost one Kiwi man in four will die before they reach retirement age.
PHO clinical advisor Dr James Peckett says too often, men were reluctant to talk about their health but when they do, they discover other men have similar experiences to their own.
“Men like to hang out, have a yarn and get to know each other. But sometimes we find it difficult to talk about our physical, mental or spiritual health. Some feel that this makes them appear weak. Or maybe we think that the bloke we are chatting with doesn’t want to know about these matters. Some feel that they are not worth the discussion.
“But when men come together and share their journey, we find out that we are not alone and that those around us do actually care.“
James says by proactively holding activities that encourage healthy conversations, the group’s participants can increase their resilience and that of the organisations with which the PHO partners.
Our Performance
Our new framework
We’re proud of the achievements and performance of the organisation this year. The team has been focussing on our top priorities of Māori health and wellbeing, and equity.
We’re constantly evolving and looking at ways to track our progress. Our new framework model covers four levels of monitoring and measuring:
We want to monitor whether the design and development of services for Māori are undertaken in partnership with the Tino Rangatiratanga Iwi Commissioning Agency (TICA) being established. Reporting should describe how the proposed services target Māori needs and why the design approach is relevant to Māori.
We are seeking to ensure that services are being delivered in partnership and in a locality model; that best endeavours are being made to share relevant data and other information to support coordination and integration. That information is also being used transparently to support common improvement, which may improve General Practices, Māori providers and other community providers.
We want assurances that services are accessible, relevant to and taken up by whānau and that providers from across the system are building their own skills and capacity to support Māori health and wellbeing. Note – it is important that there are independent and effective means to assess whānau perspectives on service delivery.
We should be measuring if all this activity makes a difference. There are many ways to measure impact, and this will depend on the needs targeted and the services delivered. Measuring impact can be difficult but that does not mean it should not be thoughtfully attempted. These measures should be designed in collaboration with the Tino Rangatiratanga Iwi Commissioning Agency (TICA).
+ 704
67%
Māori women screened for cervical cancer
85.6%
Student contacts with School Health Services
+ 815
Comprehensive health assessments for Year 9s
72%
– 5,631
– 758
+ 3580
66.3%
Māori over 65 years who received influenza vaccinations
Western Bay of Plenty Primary Health Organisation Limited
2021-2022 Financials
Our Future Direction
The bigger picture
As we move towards Pae Ora (Healthy Futures) and delivering a better health system for Aotearoa New Zealand, we are focused on the key areas of Māori health and wellbeing, men’s health, mental health, and equity for all. Here’s how we’ve started on those journeys.
Our vision is to be courageous leaders of compassionate, connected, trusted, and innovative whānau-centred healthcare provision for our whole population.
Our direction
Health equity: Health equity is about fairness. We serve a diverse community with different levels of advantage that require different supports, resources, and approaches.
In our community: We act as a korowai (caring and protecting) through a range of supports, health services, health services, and programmes to support wellness.
Focus on wellness: We enable all people to shape their own health and wellbeing.
Our way of working
- Māori led: We are establishing an independent iwi-owned Māori commissioning agency, Tino Rangatiratanga Iwi Commissioning Agency (TICA) that works in partnership with WBOPPHO.
- Whānau and community voice: We will support TICA to engage with communities and identify local priorities for Māori health and wellness and to identify effective health and wellness initiatives for Māori.
- Partnering: We will work with TICA to agree how WBOPPHO can support the delivery of health and wellness programmes through its provider networks – and acknowledge that sometimes programmes may be delivered through channels that may not include our provider networks.
- Equity focus: We will ensure that our agreed service initiatives focus on improving equity.
- Locality-based: We will deliver services in a way that respond to local needs and consider local capacity, networks, and infrastructure.
- Connected: We will endeavour to connect data from across the network of community providers to support integrated services.
- Knowledge driven: We will use this connected information to provide feedback on progress, understand performance and to improve our services.
- Build capacity: We will develop the capacity of Māori providers and of general practice to respond to integrated wellbeing models.
- Enable equity and outcomes: Together we will create a system that responds to Māori health and wellbeing needs to deliver improved equity and outcomes.





